Subtotal: $
Checkout-

The Artificial Pancreas
-

From Scrolls to Scrolling in Synagogue
-

Computers Can’t Do Math
-

The Tech of Prison Parenting
-

Will There Be an AI Apocalypse?
-

Taming Tech in Community
-

Tech Cities of the Bible
-

Send Us Your Surplus
-

Masters of Our Tools
-

ChatGPT Goes to Church
-

God’s Grandeur: A Poetry Comic
-

Who Gets to Tell the Story?
-

A Church in Ukraine Spreads Hope in Wartime
-

Editors’ Picks: The Genesis of Gender
-

Readers Respond
-

Loving the University
-

Locals Know Best
-

Gerhard Lohfink: Champion of Community
-

When a Bruderhof Is Born
-

Peter Waldo, the First Protestant?

It’s Getting Harder to Die
When medical tech can keep us alive, families face tough choices.
By Lydia S. Dugdale
June 24, 2024
Recently I was speaking to a group of sophisticated New Yorkers about the preparation for death. Someone asked a tentative question about life support, and I quickly realized that for all their erudition, they were largely ignorant about what happens in the hospital as people approach death. As a primary care doctor and clinical ethicist, I am often in the position of helping patients and families navigate these questions in real time, sometime at the darkest time of their lives. Here, I would like to offer some thoughts that might help the reader prepare for these decisions before death is imminent.
If you ask me how I think about my own dying in our high-tech world, I tell myself this:
- Stay out of the hospital if possible.
- Avoid new devices, interventions, and procedures if possible.
- Spend your remaining days at home if possible.
- Nurture relationships with those you love.
I work in one of the most technologically sophisticated hospitals in the world; I am not anti-tech or anti-hospital. But when it comes to dying, my preference is for low-tech and at home. This assumes, of course, that either I’m very old, or I have a medical condition or set of problems that suggest death is relatively imminent. But this raises two related questions: First, how do we know how old is old enough to forgo life-sustaining therapies? And second, how do we know when death is imminent?
Taking a step back, it’s helpful to think about how people typically die in the West. The bioethicist Joanne Lynn observes that Americans usually die in one of three ways: they are relatively healthy until a previously treated disease such as cancer comes roaring back; or they have a chronic disease such as heart failure that relapses and remits, with successive relapses becoming more and more frequent until the person dies of the disease; or they live a long life and die of the accumulated assaults and annoyances of old age. (A small minority dies by accident or violence, but such deaths can’t usually be anticipated.)
In thinking about what it means to live and die well in each of these instances, Lynn might advise that those in the first category consider during their period of remission enrolling in hospice services when their cancer comes back. The second group with progressive chronic disease should develop a contingency plan for when disease progression becomes overwhelming. And the third group needs all hands on deck – including family members and community support – to manage the challenges of protracted frailty. This is the bird’s-eye view. The question then becomes how we translate this knowledge to actual decisions at the end of life.
A related question arises when, as is often the case, patients and families enter a crisis situation without having done this advance consideration – or having done it, but finding in the moment that events do not progress as they had pictured. Perhaps they are already in the hospital, deep in the throes of the many high-tech supports available, unsure how to navigate the options. In either case, recognizing and accepting the imminence of death can help patients and families find some peace as death approaches.
The Medicalization of Death in a High-Tech World
Sometimes it seems the hospital offers an interminable array of life-sustaining interventions. These are some of the most common:
Cardiopulmonary Resuscitation. When a patient is admitted to a hospital or nursing home, one of the first questions doctors ask is whether they have a “Do Not Resuscitate” order, meaning whether they do not wish for cardiopulmonary resuscitation, or CPR. When the heart stops, a person is dead. In rare instances, health care professionals can bring the patient back to life by performing chest compressions and breathing into the dead body until the heart restarts. In contrast to what’s depicted by Hollywood, CPR rarely works. It is more likely to be successful in the hospital than outside, and even when it works, most patients do not survive to hospital discharge. Their hearts stop again in fairly short order.
Additionally, the chest compressions themselves result in excruciatingly painful rib fractures, and more than several minutes of death without chest compressions can lead to irreversible brain damage. Hearts wear out with advanced age, frailty, and disease burden, which means the possibility of meaningfully restarting the heart diminishes as the years and disease progress.
Hemodialysis. When the kidneys fail, hemodialysis machines can filter the blood in their stead. Dialysis is a remarkable intervention that offers people many years of life, but it is no small undertaking. It requires three four-hour sessions per week for the rest of one’s life, absent an organ transplant. Patients must be transported to dialysis facilities and remain hooked up to the machine. The process of filtering blood can be exhausting and uncomfortable, and removing and restoring patients’ blood exposes them to infection and clotting problems.
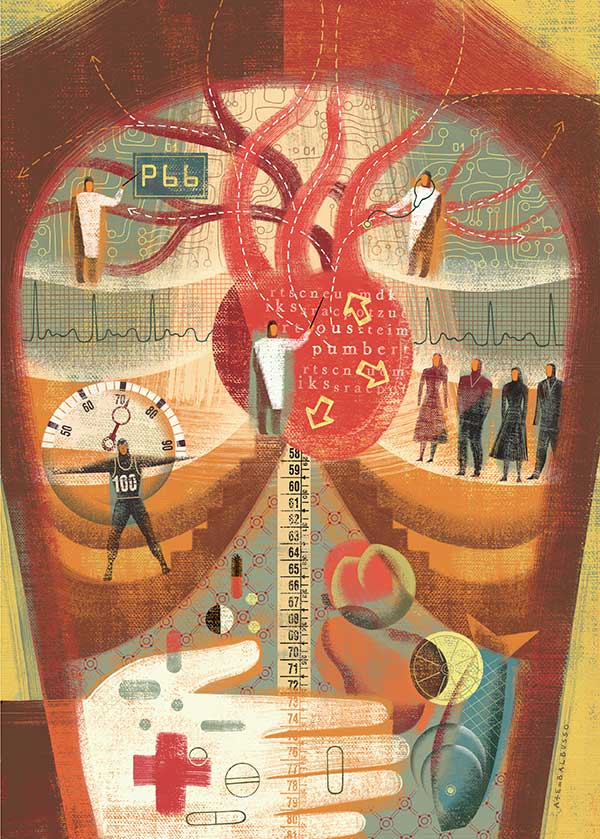
Anna & Elena Balbusso, Education, acrylic on paper and digital, 2005. ©2005 Anna & Elena Balbusso c/o theispot.
Artificial Nutrition and Hydration is especially critical when an otherwise healthy person loses the ability to chew, swallow, or absorb nutrients from the gut. A classic example might be throat cancer. During prolonged treatment, a person with throat cancer cannot swallow, and artificial nutrition and hydration prevents such a patient from dying of dehydration. The same would be true for people with advanced dementia who have stopped eating – artificial nutrition and hydration would also prevent their dehydration. However, dementia experts widely agree that by the time dementia advances to the point of not eating, such patients do not feel hungry or thirsty, and disinterest in food and drink is part of the body’s way of winding down toward death. Whereas providing artificial nutrition and hydration to the patient with throat surgery would be understood as part of treatment and indeed ethically obligatory, in the case of advanced dementia doctors generally believe that the burdens outweigh the benefits. Even though artificial nutrition and hydration are well tolerated with minimal side effects, it is always possible that the tubes or lines become dislodged, disconnected, or infected.
Chemotherapy. Modern medicine might best be characterized by an imperative to treat. If a treatment is technically available, we should offer it, even if its effectiveness is virtually nil. This is especially true for cancer chemotherapy. When patients are diagnosed with cancer, it is critical to understand the chance of remission or cure from any given treatment. First- and second-line chemotherapies might have good outcomes, but does the third- or fourth-line? The answers vary by type of cancer, and patients and their families must clearly understand the benefits and harms of various chemotherapies before agreeing to them. Not only do about a quarter of cancer patients declare bankruptcy or lose their homes from the high cost of treatment, but also studies show that in some cases patients who forgo chemotherapy report a better quality of life and even live longer. Thus, chemotherapy is not always the answer.
Organ Transplantation. When patients on dialysis receive a transplanted kidney, or when people dependent on heart-pumping devices receive a transplanted heart, they often describe “getting my life back.” And indeed, this can be the case. Many people who receive transplanted organs do very well. But many do not. It can take months to recover from surgery. Furthermore, patients must take medicines that suppress the immune system to prevent their bodies from rejecting a foreign organ, which increases their risk of life-threatening infections. Between potential hospitalizations from complications and follow-up doctor appointments, some don’t return to their former lives but instead settle into new forms of highly medicalized living.
Forgoing Treatments and Assessing Death’s Imminence
The fact that all these interventions are marvelous yet potentially troublesome suggests that we have wiggle room in choosing when to pursue them. Such wiggle room is legal as well as ethical. In Cruzan v. Director, Missouri Department of Health (1990), the US Supreme Court assumed that adults of sound mind have the right to refuse lifesaving artificial nutrition and hydration – a view that has been upheld and extended in subsequent decisions to include a right to refuse any unwanted medical intervention.
Legality aside, most people feel that it is ethical to withdraw or refuse life-sustaining treatments, especially when the burdens of such interventions outweigh the benefits. Imagine a scenario in which Jack’s lungs fail and are unlikely ever to recover. He requires a mechanical ventilator to do the work of the lungs and is able to go home with the machine ventilating through a tracheostomy hole in his neck. He lives this way for some years, but as complications accumulate and he grows frailer, he decides that he no longer wants to live on the machine. His medical specialists are certain that he will die relatively quickly without it, and together they plan to withdraw the ventilator while providing medication to mitigate Jack’s inevitable sensation of air hunger.
An initial response to such a scenario is to say, “Wait a second. Aren’t you killing him by removing the ventilator?” But the answer is that the act of removing the ventilator is not the cause of his death; rather, his death is caused by the progression of his underlying disease. Although Jack is dependent on the ventilator, there is no guarantee that he will die the split second the ventilator is removed. (And even if there were a guarantee, as, perhaps in advanced Lou Gherig’s Disease or ALS, the ventilator removal is not considered the cause of death but in fact the progressing ALS is.) In fact, most medical professionals can tell stories of removing a ventilator with the expectation that the underlying disease will quickly consume the life of the patient, but the patient goes on to live for a surprising length of time, from days to years. What this means is that removing life support is not killing. Rather it allows the patient’s disease to follow its natural progression to the end.
Medical ethicists also distinguish between withholding life-sustaining interventions and withdrawing them. Most of us ethicists believe that these are morally equivalent acts, but we recognize that they might feel different emotionally. Take the example of Jack again. Jack’s lungs fail, he needs a ventilator, but he refuses. Instead, his doctors provide medication to subdue his feelings of air hunger, and he eventually dies, having never gone on the ventilator. Alternatively, Jack goes on the ventilator for some years until, for whatever reasons (accumulating medical problems, advanced frailty, or dementia, etc.), he or his health care agent asks to have it removed. It is at that point that his medical team rallies to focus on comfort measures. In both instances, decisions are made at specific points to forgo life-sustaining interventions. Even though they are ethically equivalent, it can feel emotionally weightier – more like killing – to remove the ventilator he’s lived with for years and to which Jack and his family have grown accustomed.
I noted at the outset that my own preferences for being at home and focusing on comfort over medical interventions hinge on my being either very old or having a medical condition or set of problems that suggest death is relatively imminent. But what about removing life support for someone young, without many medical problems, who is expected to recover? Although it is legal for a young adult of sound mind to refuse ventilator support for, say, a life-threatening exacerbation of her asthma, most people would not think it ethical to allow a young, otherwise healthy woman to die of an entirely treatable disease. One’s age, death’s imminence, and accumulated medical problems matter to the question of when it becomes ethical to remove or withhold life-sustaining therapies. How, then, do we know when it’s time?
Age cutoffs are not the answer. They are too simplistic. Surely we all know eighty-somethings living active, independent lives and sixty-somethings who are very ill and need constant care. In my book The Lost Art of Dying, I propose we learn a concept that has been floating around the halls of geriatric medicine: frailty risk assessments.
Probably the most widely used assessment today consists of five components, and nearly all of us can learn to use it. People over the age of sixty-five are considered “frail” if three or more of the following ring true:
- Unintentional weight loss of ten pounds or more in the last year
- Feelings of exhaustion
- Physical weakness, measured by checking handgrip strength with a dynamometer (or, can Grandma hold her coffee cup?)
- Slow walking speed, measured as requiring six or seven seconds to walk fifteen feet
- Low physical activity
Of course, many factors other than age increase risk of frailty, including smoking and mental illness. The frailty risk assessments apply to these other groups as well.
The point here is that the frailer people become, the less likely they are to “bounce back” from surgery or a prolonged hospital stay. When Grandma’s clothes have become baggy, she hardly gets out of bed, and she no longer engages in much activity, we need to think twice about the benefits of CPR, hemodialysis, or artificial nutrition and hydration. Delaying the moment of Grandma’s natural death because we ourselves are so afraid of death is hardly the way to care well for our aging loved ones. As a friend said to me recently, “My mother keeps wanting to discuss her funeral plans, and I’ve been trying to avoid it. I realize now how selfish I’ve been.”
Dying Well Today
Dying well today starts with open and honest conversations – not only with loved ones and spiritual or religious communities, but also with medical professionals. The wisdom of earlier generations and especially the ars moriendi (“art of dying”) body of literature is that we die the way we live. People who want to be known in their dying and after death as patient, loving, and kind must cultivate patience and lovingkindness over the course of their lives.
But it’s a bit more complicated with health care. Because even if we’ve dutifully visited the doctor and had all our age-appropriate cancer screenings, there may come a point where it makes the most sense to shed such corporeal preoccupations with health care for the sake of a future unencumbered by the trappings of medicalization, a future in the environment of our choosing, and where we are surrounded by those we love. In the case of medicalization, it might not make sense to die the way we lived.
For all the marvels of our high-tech lives, we must insist whenever possible on a low-tech exit – at least that’s what I believe, having seen death up close many times. In my own case, I am hopeful that when death draws nigh, and especially if I am unable to advocate for myself, my family and doctors will jointly and wisely determine when interventions pose more burden than benefit. I am hopeful that years of conversation about the need to prepare well for death – medically, communally, and spiritually – translate into a sober and realistic assessment of the medical facts and a willingness to allow me to return to the very low-tech dust from which I came.
Already a subscriber? Sign in
Try 3 months of unlimited access. Start your FREE TRIAL today. Cancel anytime.






























Melissa Olivia
Thank you Lydia. This was beautifully written and spoke to my heart. My family just went through this and I’m sharing with others to help them navigate this process. We need to normalize death and grant people the dignity they deserve.
VD
“Professional ethicist.” Lol. In med school we always laughed at these self appointed ethicists. They were usually slightly less ethical than the average attending and often had seriously messed up personal lives.
Nigel Parrott
My wife Anne died in the year2000 of M.N.D at the age of 35. As Christians we did not believe in euthanasia as this is to take God's place. But to allow it to be the Lord's timing not man's, palliative care only. However this was not easily acceptable by the medical profession ,and we had to fight them all the way. As Christians we need to advocate for people to be allowed to die , without unnecessary life extension. As a foot note Anne died at home with me and our son peacefully.
gordon hadlow
This was an excellent article, giving many considerations in the realm of death and dying. It is extremely important, as the article says, for families to discuss these factors.
Andree Koehler
Thank you so much, Lydia -- my mother was on dialysis for many years and when her health declined to the point that she wasn't eating or drinking and I as her only child had to decide whether she would receive external nutrient, I asked questions. It was terribly hard and got harder when I spoke with her companion, who himself was struggling with her poor health. In the end, after I truly heard the answers to my questions about the challenges of saying yes to this type of nourishment for someone in my mom's condition, I thought about her quality of life. In the end, she went on hospice and rallied some after the medications were stopped. One of her doctors called me and shared with me how wonderful she thought my mom was (having treated her for several years and through multiple hospitalizations) and that I had made the right decision. It meant more to me than any other exchange I think I've had with a medical professional. It is difficult, but as you wrote, being able to support someone in leaving this mortal life well is the best thing we can do, especially if they are not in a full position to make that decision themselves. My mom had thought ahead and did have an advance directive, but in the moment it's sometimes difficult to know where those documents are. In my mom's situation, her companion and I found them afterward and were so relieved to know that we had acted according to her wishes.
Laura
Thank you for this article. I was the health surrogate for my father. He made sure I knew that he did not want to stay alive and in fact told me shortly after going into long term skilled care that he knew his time was coming soon (he was 89) even with no real underlying issues. We had several conversations and I promised I would not allow anyone to revive him when that time came. And so it came less than two months later. I had educated myself enough to know when he slowly stopped eating and recognized other signs that his body was getting ready to pass. When he was taken to the hospital unresponsive I made sure the staff and doctors knew he had a DNR and that no actions should be taken. He passed peacefully three hours later. I was glad I could do this for him. He died on Junteeth of 2023, the day the slaves were set free. He was also set free that day.